Valvuloplastie mitrala cu balon / Tratament stenoză mitrală hipertensiune pulmonara
| Anestezie | locală/generală |
| Durată procedură | 1-3 h |
| Durată spitalizare | 24 h |
Cuprins
- Generalități despre valvuloplastia mitrala cu balon
- Valvuloplastia mitrală cu balon
- Cauze:
- Cele mai frecvente simptome ale stenozei mitrale sunt:
- Cum te pregătești pentru valvuloplastia mitrală?
- Cât durează internarea?
- Riscuri valvuloplastie mitralăcu balon
- Ce se întâmplă în timpul procedurii de valvuloplastie mitrală
- Hemostaza
- Ce dispozitive medicale sunt folosite?
- Ce se întâmplă după procedură?
- Ce trebuie să faci după ce ieși din spital?
Generalități despre valvuloplastia mitrala cu balon
Valvuloplastia este efectuată, în anumite circumstanțe, pentru a trata o valvă stenozată.
Inima funcționează ca o pompă musculară. Are patru cavități: două cavități superioare, numite atrii și două cavități inferioare, numite ventriculi. Atriul drept primește sângele venos (neoxigenat) din corp, pe care îl transmite mai departe în ventriculul drept, iar de aici, prin artera pulmonară, sângele ajunge la nivel pulmonar și este oxigenat. Mai departe, sângele oxigenat ajunge prin venele pulmonare în atriul stâng și de aici, în ventriculul stâng apoi, prin aortă, ajunge în tot corpul.
Pentru a asigura curgerea normală a sângelui, între atrii și ventriculi există valve, astfel:
• valva tricuspidă – între atriul și ventriculul drept
• valva pulmonară – între ventriculul drept și artera pulmonară
• valva mitrală – între atriul și ventriculul stâng
• valva aortică – între ventriculul stâng și aortă.
Afectarea valvelor poate duce la afectarea curgerii normale a sângelui, cu anumite consecințe. O valvă disfuncțională poate fi îngustată (stenotică), fie insuficientă (regurgitantă).
Valvuloplastia mitrală cu balon
Indicațiile de valvuloplastie includ:
- stenoza mitrală severă (aria valvei calculata ecografic<1.5cmp), morfologie favorabil, absența contraindicațiilor ( prezența trombilor în atriul stâng sau regurgitare mitrală importantă).
- stenoza mitrală severă, asimptomatică, asociind hipertensiune pulmonară (presiunea în artera pulmonară în repaus >50mmHg sau la efort>60mmHg), cu morfologie favorabilă a valvei.
- stenoza mitrală severă cu valvă calcificată la pacienții cu risc mare operator, dacă sunt prezente stenoză severă și semne de insuficiență cardiacă. În anumite situații chiar și pacienții cu risc scăzut pot fi considerați pentru această metodă de corecție.
- stenoză moderată care asociază hipertensiune pulmonară
- stenoză severă care asociază fibrilație atrială nou instalată.
- stenoză severă, chiar dacă morfologia valvulară nu este cea adecvată, în scop paleativ.
Cauze:
Principala cauză a stenozei mitrale o reprezintă afectarea reumatismală a valvei în cadrul reumatismului articular acut (afecțiune dată de streptococul beta hemolitic de grup B), manifestare care se poate produce chiar și la ani de la infecția acută.
Stenoza mitrală are și alte cauze: pacienții dializați, sindrom carcinoid, fibroelastoză eozinofilică endomiocardică și poate fi și congenitală.
Simptomele sunt variate, de la oboseală și amețeală, la durere în piept și respirație dificilă. Unii pot simți palpitații, în timp ce alte persoane sunt complet asimptomatice.
Cele mai frecvente simptome ale stenozei mitrale sunt:


Cum te pregătești pentru valvuloplastia mitrală?
 1. Vei face un examen clinic complet
1. Vei face un examen clinic complet 2. Vei face o radiografie toracică
2. Vei face o radiografie toracică 3. Vei face un set complet de analize de sânge
3. Vei face un set complet de analize de sânge Vei elimina orice potențial focar infecțios: infecții ORL, stomatologice, etc
Vei elimina orice potențial focar infecțios: infecții ORL, stomatologice, etc
Cât durează internarea?
Valvuloplastia mitrală cu balon are avantajul unei recuperări rapide și a unei scurte durate de spitalizare. Durata de spitalizare este, în general, de două zile, dacă evoluția post intervenție este favorabilă și fără complicații.
Riscuri valvuloplastie mitralăcu balon
Complicațiile sunt rare și sunt evitate printr-o pregătire și supraveghere corespunzătoare. Complicațiile posibile includ:
• reacții alergice la administrarea substanței de contrast, inclusiv insuficiență renală
• reacții la compușii anestezici
• fistule arteriovenoase la locul puncției
• sângerări, hematom la locul puncției
• febră
• cefalee (durere de cap), migrenă
• infecții a locul puncției
• embolie gazoasă
• aritmii cardiace
• accident ischemic tranzitor sau accident vascular cerebral – risc redus prin efectuarea de rutină a ETE, pentru e exclude prezența trombilor.
• regurgitare mitrală nouă sau agravarea unei regurgitări preexistente
• ruptura valvei – necesită intervenție chirurgicală deschisă
• deces <1% din cazuri; risc mai mare la vârstnici sau la cei cu stare extrem de gravă la momentul intervenției
• perforație cardiacă <1%
• defect septal atrial iatrogen – în cazul abordului anterograd; se închide de obicei în câteva săptămâni postprocedural. (poate persista în 2% din cazuri).
• până la 20% dintre pacienți pot redezvolta stenoza mitrală.
Ce se întâmplă în timpul procedurii de valvuloplastie mitrală
Procedura de valvuloplastie se efectuează în sala de angiografie.
Se pregătește locul de abord prin îndepărtarea părului din zona inghinală, se efectuează asepsia locală și se administrează tratament anticoagulant. Pacientul este monitorizat pe tot parcursul intervenției.
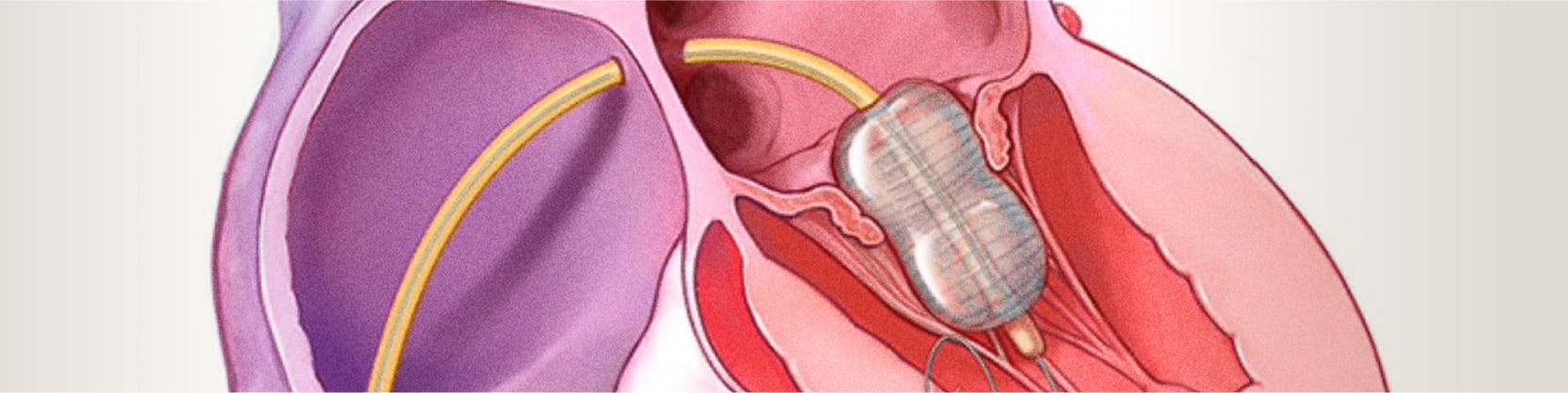
Medicul intervenționist va efectua mici incizii la nivelul canalului inghinal ( la rădăcina coapsei) pentru a vizualiza artera femurală. La acest nivel, se va introduce o teacă, ulterior pe teacă se introduc catetere până la nivelul inimii. Se injectează substanța de contrast și se efectuează angiograme repetate, pentru a vizualiza stenoza și a verifica locul cateterului. Cateterele pot fi plasate și înaintate fie pe cale venoasă (abord anterograd – metoda cea mai utilizată), fie pe cale arterială (abord retrograd).
La injectarea substanței de contrast, pentru scurt timp, se poate descrie o senzație de caldură locală, gust metalic, scurtă durere de cap. Pe cateterul poziționat la nivelul stenozei se avansează un alt cateter cu balon, până în apropierea stenozei. Balonul va fi umflat la nivelul îngustării, care va fi mărită progresiv, îndepărtându-se astfel stenoza. Ulterior, balonul se dezumfla și este îndepărtat. Pot fi necesare umflări succesive ale balonului, pentru a obține rezultate optime.
Hemostaza
După terminarea procedurii se scot cateterele și tecile arteriale, iar la locul de puncție se realizează compresia arterei folosite ca abord. Pentru a se obține compresia, se pune un pansament compresiv ce trebuie păstrat timp de 24 de ore pentru a se evita sângerările.
În ambele cazuri de abord, pacientului i se va indica să păstreze repaus la pat. În anumite situații, există indicația de a monta un sistem hemostatic la nivelul puncției femurale. Acesta se montează în sala de angiografie, imediat după terminarea intervenției. AngioSeal este mic dop de colagen și se introduce în interiorul arterei femurale. Acesta are ca efect obținerea hemostazei în doar două ore. Astfel, pacientul își poate mișca piciorul în voie și se poate ridica din pat.
Ce dispozitive medicale sunt folosite?

Ce se întâmplă după procedură?
 1. Vei fi transferat în salonul de recuperare
1. Vei fi transferat în salonul de recuperare 3. Vei primi un tratament medicamentos
3. Vei primi un tratament medicamentos 4. Vei fi supus mai multor examene clinice și investigații
4. Vei fi supus mai multor examene clinice și investigații
Ce trebuie să faci după ce ieși din spital?
Dacă ai fost supus unei proceduri de valvulopastie mitrală cu balon, trebuie să revii la controlul cardiologic la o lună, la trei luni și apoi o dată la șase luni, în funcție de evoluție. Imediat după externare vei face recuperare fizică. Vei urma un tratament medicamentos la indicația medicului.
Locații MONZA ARES în care se efectuează Valvuloplastie mitrala cu balon / Tratament stenoză mitrală hipertensiune pulmonara
Procedurile Noastre
- Investigații cardiologie
- Electrocardiograma - ECG / EKG
- Consult Cardiologic
- Ecocardiografie / Ecografie cardiacă
- Ecografie doppler carotidiana
- Ecografia doppler de artere / vene
- Holter EKG - Monitorizarea ritmului inimii 24H
- Holter TA - Monitorizare tensiune arteriala
- Ecografia cu dobutamină / Ecografia de stres
- Test de efort / Ergometrie
- Ecocardiografia transesofagiană
- Programare Stimulator Cardiac
- Evaluare si control cardiovascular complet post COVID-19
- Ecografia cu bule / cu substanță de contrast
- Ecocardiografia speckle tracking
- Consultație diabetologie
- Indice Gleznă/Braț
- Consultație cardiologie pediatrică
- Programul de readaptare cardiacă/ recuperare cardiovasculară post COVID-19
- Investigații neurologie
- Bolile valvelor și ale vaselor inimii
- Coronarografie - Angiografie coronariana / Diagnostic angina pectorala
- Angioplastie coronariană cu stenturi / Tratament angină pectorală ischemie cardiacă
- Tratament stenoză aortică – TAVI – Implantare valvă aortică
- Tratament insuficiență mitrală - MitraClip
- Valvuloplastie mitrala cu balon / Tratament stenoză mitrală hipertensiune pulmonara
- Revascularizarea ocluziilor coronariene cronice totale (CTO)
- Rotablație coronariană - Tratament angină pectorală (artere calcifiate)
- Procedura JetStream – sistem de aterectomie pentru dezobstrucția arterelor sever calcifiate
- Terapia Shockwave / Tratament boala cardiacă ischemică – artere calcifiate
- Implantare de stent Flow Reducer / Tratament angina pectorala rezistenta la medicație
- Chirurgia valvei mitrale / Operatie chirurgicala insuficienta mitrala
- Bypass aorto-femural și femuro-popliteal / Operatie pentru ateroscleroză
- Bypass aorto-coronarian / Operatie chirurgicala pentru angină pectorală
- Aritmii cardiace
- Ablatie fibrilatie atriala | Tratament fibrilatie atriala
- Ablatie flutter atrial / Tratament flutter atrial
- Ablatie tahicardie jonctionala / Tratament tahicardie joncțională
- Implantare stimulator cardiac / Tratament dereglări de ritm cardiac
- Implantare Defibrilator cardiac / Corectarea prin șoc electric a ritmului inimii
- Sindrom WPW | Wolff-Parkinson-White
- Procedura Watchman pentru fibrilatia atriala / Tratament preventiv AVC in fibrilatia atriala
- Tahicardie | AVNRT | Tahicardia prin reintrare in nodul atrio-ventricular
- Monitorizarea electrocardiografica pe termen lung | LOOP RECORDER
- Studiu electrofiziologic / Identificarea zonelor de aritmie cardiaca
- Cardioversie electrica – restabilirea ritmului normal al inimii
- Bradicardie | Tratament aritmie cardiaca lenta
- Ablatia prin radiofrecventa | Crioablatia / Tratament tahiaritmii cardiace
- Defecte (malformații) cardiace din naștere
- Bolile vaselor de sânge
- Embolizare hemoroizi / Tratament minim invaziv hemoroizi
- Angiografia generală / Diagnostic artere blocate
- Anevrismul de aorta / Tratament aorta dilatata
- Implantare de stent graft - Disecție de aortă de tip B
- Angiografia de artere mezenterice - angioplastie cu balon și stent / Diagnostic si tratament ingustare vase de sange sistem digestiv
- Angiografia de artere periferice - angioplastie cu balon si stent / Diagnostic si tratament ingustare vase de sange maini si picioare
- Angioplastia de artere renale / Tratament ingustare vase de sange rinichi – reducere hipertensiune arteriala
- Angioplastie artere subclavii / Tratament ingustare vase de sange gat
- Implantare de filtru de vena cava inferioara / Preventie embolie pulmonara
- Denervarea arterelor renale / Tratament minim invaziv hipertensiune arterială rezistenta la tratament
- Angioplastie venoasa cu balon si stent
- Fibroid Center
- Embolizare fibrom uterin / Tratament minim invaziv fibrom uterin
- Consultatia ginecologica
- Ecografia transvaginala / endovaginala
- Test HPV (Papilloma Virus Uman)
- Test Babes-Papanicolau
- Ginecologie - Trichomonas Vaginalis
- Ginecologie - Candidoza vaginala
- Colposcopie
- Electrorezectia / Prelevare țesut col uterin
- Ecografia de morfologie fetala - Trimestrul I
- Ecografia de morfologie fetala - Trimestrul II
- Ecografia de morfologie fetala - Trimestrul III
- Boli oncologice si tratamente tumorale
- Bolile valvelor și ale vaselor inimii la copii
- Embolizare hemangiom / Tratament minim invaziv tumori benigne
- Fistula arterio-venoasa coronariana / Tratament legatura anormala artera si vena
- Fistula arterio-venoasa pulmonara / Tratament legatura anormala artera si vena pulmonara
- Stenoza pulmonara periferica / Tratament ingustare artera pulmonara
- Valvuloplastie pulmonara cu balon / Tratament ingustare valva pulmonara
- Boli ale aparatului genital masculin
- Boli cerebrale și ale coloanei vertebrale
- Anevrismul cerebral / Tratament durere de cap, paralizii preventie AVC
- Angioplastie carotidiana / Tratament boala carotidiana, atac ischemic vascular, AVC
- Discectomie cervicala cu DiscoGel / Tratament hernie de disc cervicala
- Malformatii arterio-venoase cerebrale / Tratament hemoragii cerebrale
- Nucleoplastie / Tratament hernie de disc
- Vertebroplastie / Tratament dureri coloana vertebrala fracturi de compresie
- Discectomie cu alcool
- Infiltrații transforaminale
- Boli ale articulațiilor

