Insuficiența cardiacă
Articol medical scris de către Dr. Mihaela Rugină, Cardiologie clinică la MONZA ARES Bucuresti
Distribuie:
Cuprins
Despre insuficienta cardiaca
Insuficiența cardiacă apare atunci când mușchiul inimii nu poate pompa suficient sânge. Mai multe afecțiuni pot cauza insuficiența cardiacă. Printre cele mai frecvente sunt: afecțiuni ale arterelor inimii ( arterele coronare sunt îngustate de depuneri de calciu și alte materiale din sânge) și hipertensiunea arterială.
Nu toate cauzele insuficienței cardiace sunt reversibile, dar tratamentul specific poate duce la îmbunătățirea semnelor și simptomelor de insuficiență cardiacă. El poate îmbunătății calitatea vieții și poate scădea numărul de spitalizări.
Schimbarea stilului de viață, incluzând exercițiu fizic regulat, dieta hiposodată, scădere ponderală, dar și controlul factorului stres, poate contribui la îmbunătățirea calității vieții.
Cea mai bună cale de a preveni insuficiența cardiacă este de a controla condițiile care duc la această afecțiune. De exemplu, boli ale arterelor coronare, hipertensiunea arterială, diabetul zaharat, obezitatea. Insuficiența cardiacă este o condiție care poate evolua cronic sau acut (fie ca prima manifestare, fie ca acutizare (agravare) a unei evoluții cronice).
Ai putea suferi de insuficiență cardiacă dacă ai simptomele:









Când este cazul să apelezi la un doctor?
Atunci când apar simptome care sugerează insuficiența cardiacă. În cazuri severe se va apela serviciul de urgență. Astfel de situații sunt:
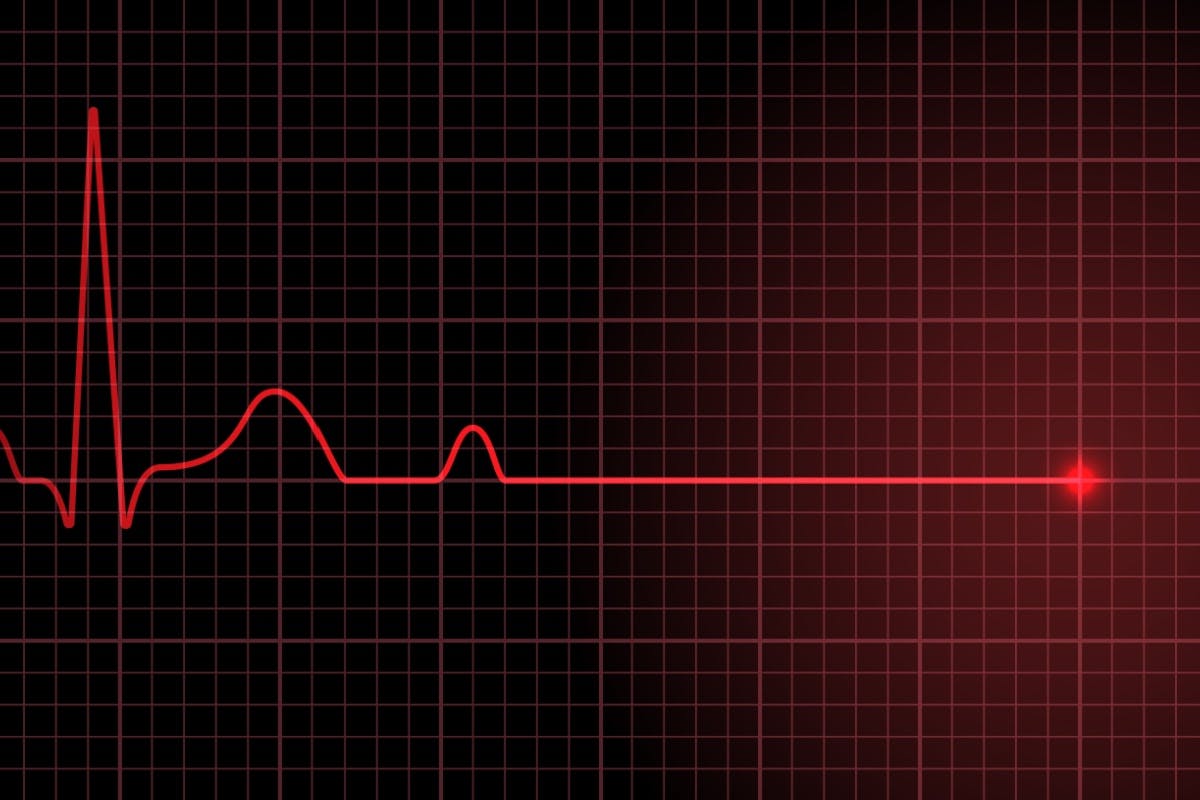
• durere în piept (angină)
• pierderea stării de constiență (sincopa), oboseală, slăbiciune extreme
• bătăi cardiace rapide, regulate sau neregulate, eventual asociate cu dispnee, angină, sincopă
Toate aceste simptome pot apărea în contextul insuficienței cardiace ca și agravare a acesteia. Ele pot fi asociate și cu alte afecțiuni, unele amenințătoare de viață. De aceea, important este să apelezi serviciul de urgență și să fii evaluat cât mai repede de un medic specialist, pentru a stabili cauza lor.
Dacă ai diagnosticul de insuficiență cardiacă și unele semne sau simptome se agravează sau apar noi manifestări, probabil insuficiența cardiacă se agravează sau nu răspunde la tratamentul urmat. În acest caz ar trebui sa te adresezi medicului tău.
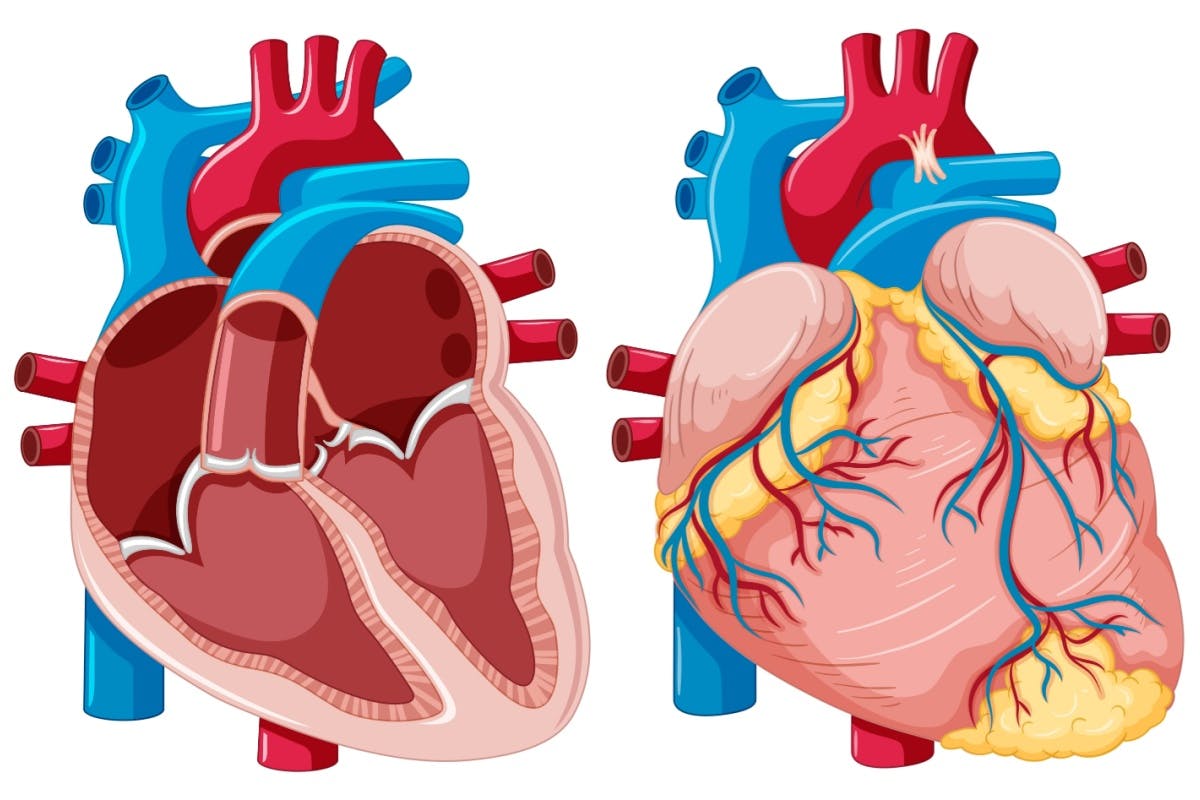
Cauze ale insuficienței cardiace
Insuficiența cardiacă se dezvoltă cel mai frecvent ca și complicație a afectării inimii în diverse boli. În timp, inima nu mai poate pompa suficient sânge pentru a face față cererilor organismului. Inițial, la eforturi progresiv mai mici, ulterior și în repaus. Principala activitate de pompă e menținută de către ventriculul stâng. La fiecare contracție trimite în aortă o anumită cantitate de sânge necesară bunei funcționări a întregului organism. Ventriculul stâng poate suferi diferite modificări în timp. Spre exemplu, devine mai rigid, contracția lui fiind astfel afectată. Sau umplerea lui cu sânge scade, ceea ce duce, evident, la scăderea cantității de sânge pe care el o poate trimite în corp. De asemenea, mușchiul inimii poate suferi, devine “slăbit” și “obosit”. Secundar efortului imens de a mentîține funcția normală a inimii, în timp ventriculii se pot dilata, până la un punct când inima nu mai poate pompa sânge suficient în corp.
Uneori, insuficiența cardiacă se complică cu acumulare de lichid în diverse zone ale corpului. Cel mai frecvent la nivelul picioarelor, dar și la nivel abdominal sau la nivelul plămânilor (edem pulmonar).
Tipuri de insuficiență cardiacă
Insuficiență cardiacă stângă
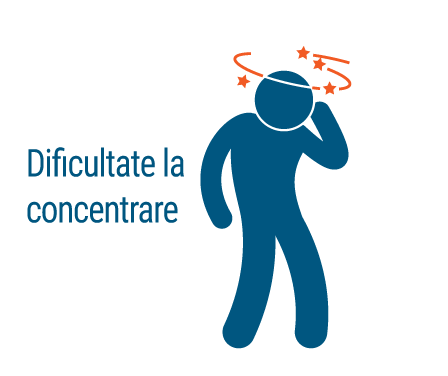
Lichidul poate staționa la nivelul plămânilor, ducând la dispnee, tuse cu hemoptizie (mici striuri de sânge), scade debitul cardiac (cantitatea de sânge expulzată de ventriculul stâng în aortă) și apar semne ale scăderii acestuia, precum: oboseala, slăbiciune, astenie, scăderea capacității de efort, amețeli/sincope, scăderea capacității de concentrare și a atenției, scădere ponderală, anemie și carențe nutriționale, paloare/cianoză (tegumente și mucoase vineții – de exemplu buze, unghii), transpirații, afectarea funcției renale.
Insuficiență cardiacă dreaptă
Lichidul poate stagna în abdomen, membre inferioare – apar edemele la nivelul picioarelor, ulterior și la nivelul peretului abdominal, stază la nivel hepatic, cu durere secundară, lichid de ascită, meteorism abdominal (balonare), greață, anorexie (lipsa apetitului), icter/cianoză.
Insuficiență sistolică
Atunci când contracția ventriculului stâng este afectată și nu mai poate îndeplini funcția de pompă.
Insuficiență cardiacă diastolică (denumită și insuficiență cardiacă cu fracție de ejecție normală)
În acest caz, ventriculul stâng este rigid și nu se poate relaxa eficient (între două contracții ventriculul se relaxează, lucru care permite umplerea lui cu sânge; atunci când relaxarea este afectată, va scădea umplerea) și pentru a funcționa normal ca și pompă, el va depune un efort suplimentar, care însă, în timp, duce la epuizare și la disfuncție de tip sistolic.
Oricare dintre afecțiunile următoare poate duce la insuficență cardiacă – unele dintre ele pot fi prezente fără niciun simptom.
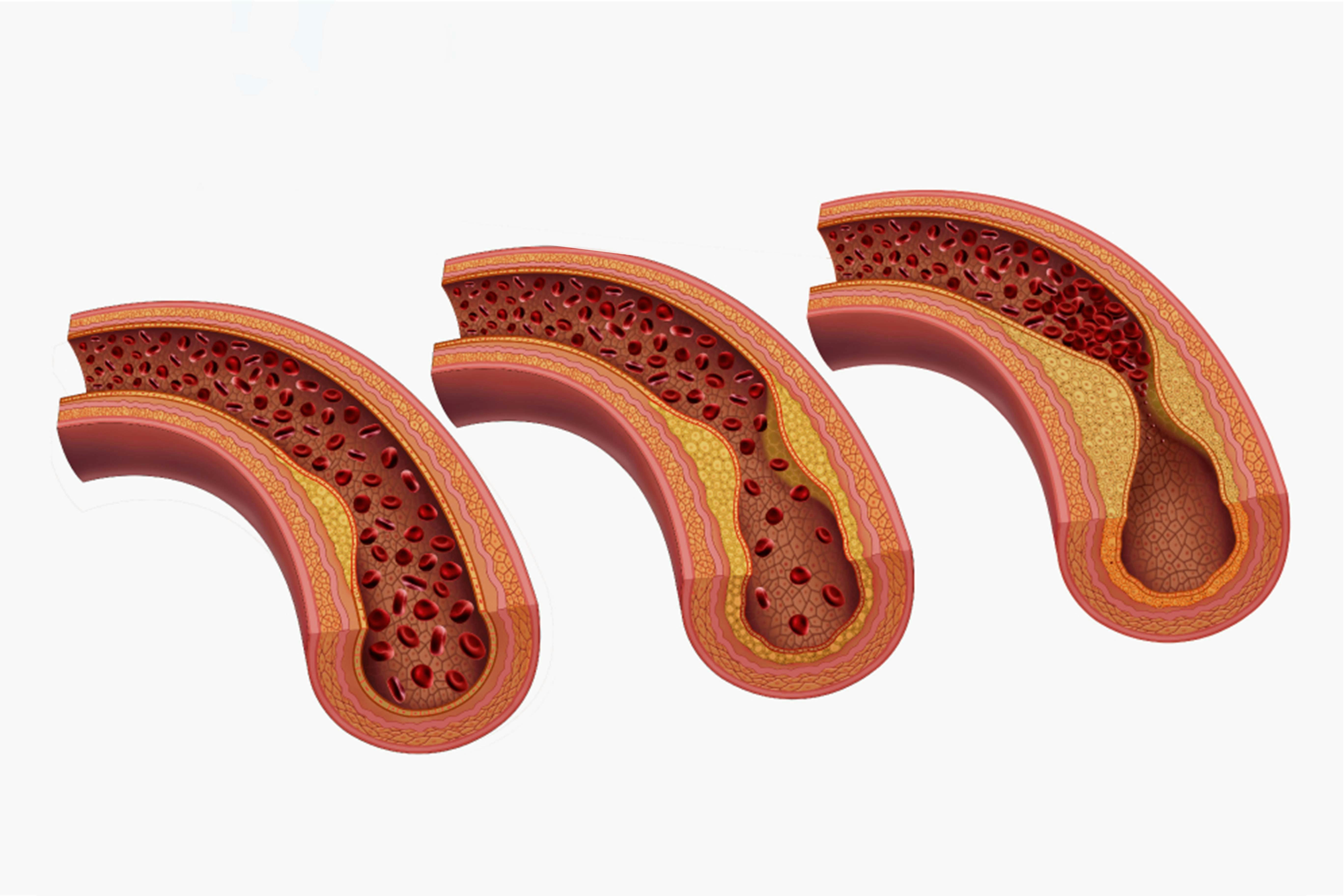
Boli ale arterelor coronare – infarctul miocardic:
– afectarea coronariană este forma cea mai frecventă de boală cardiacă. De asemenea, cea mai frecventă cauza de insuficiență cardiacă. Coronarele sunt artere care vascularizează inima. În timp, ele se pot îngusta, mai mult sau mai puțin, din cauza depunerilor de colesterol. Atunci când îngustările sunt severe, sângele va circula deficitar în acea porțiune. Acest lucru va duce la scăderea cantității de sânge la nivelul mușchiului vascularizat de vasul respectiv. Mușchiul va suferi de lipsa de oxigen (condiție numită ischemie). Uneori, aceste îngustări permit circulația sângelui suficient pentru a asigura un minim necesar sanguin. Din păcate nu suficient pentru a se îndeplini o funcție de pompă. Atunci când unul sau mai multe vase sunt închise complet, se produce infarctul miocardic, care poate avea consecințe severe (inclusiv decesul).
Hipertensiunea arterială
– tensiunea (presiunea) arterială reprezintă forța cu care inima pompează sânge în artere. Dacă această presiune este crescută, inima trebuie să depună un efort mai mare pentru a asigura circulația sângelui în artere. Acest lucru face ca, în timp, mușchiul inimii să sufere modificări adaptative. Inițial, modificările permit funcția normală, dar în timp, duc la insuficiența lui.
Afectări valvulare
– valvele cardiace mențin circulația sângelui în direcția normală. Afectarea valvulară (dată de un defect cardiac, boli coronariene, infecții cardiace) forțează inima să “muncească” mai mult pentru a menține fluxul de sânge necesar. Pe de altă parte, diagnosticate în timp util, aceste afecțiuni pot beneficia de tratament optim chirugical sau intervențional, prevenindu-se astfel deteriorarea ireversibilă.
Afectarea mușchiului inimii (cardiomiopatie)
– întâlnită în infecții, consum de alcool sau de alte toxice ( medicamente de tipul chemoterapicelor, droguri – cocaina). Există și afecțiuni determinate genetic: cardiomiopatia hipertrofică. Aceasta constă în îngroșarea mușchiului inimii, respectiv cardiomiopatia dilatativă – care presupune slăbirea mușchiului inimii și dilatarea cavităților acesteia.
Miocardita
– reprezintă inflamația mușchiului cardiac, frecvent fiind cauzată de infecții virale, poate duce la insuficiență cardiacă stângă.
Defecte cardiace congenitale
– supun inima unor eforturi mai mari în timp pentru bună funcționare, putând determina insuficiență cardiacă.
Aritmii
– determină un ritm cardiac prea rapid, ceea ce afectează umplerea ventriculară și determină un efort suplimentar cardiac pentru menținerea funcției de pompă. În timp, are același efect de epuizare, ca și în cazul afecțiunilor descrise anterior. Pe de altă parte, și un ritm cardiac scăzut poate avea aceeași consecință, prin expulzia unei cantități de sânge insuficiente.
Alte afecțiuni
– boli cronice precum diabetul zaharat, disfuncții tiroidiene (fie hiper – , fie hipo – tiroidismul), hemocromatoză ( cantitate crescută de fier în orgasnism), amiloidoza (depunere de lanțuri de proteine), deficit de vitamina B1 (boala beri-beri), tulburări respiratorii (de ex. apnee de somn)
Tratamente
Insuficiența cardiacă este o condiție cronică care necesită management pe termen lung. Cu un tratament corect și complet, simptomele pot fi mult îmbunătățite și o parte din afectare să fie recuperată. Un tratament corect poate duce la creșterea calității vieții, la scăderea numărului de spitalizări, la creșterea duratei de viață. În plus, în anumite situații tratamentul cauzei duce la corecția insuficienței cardiace. Spre exemplu, corecție în caz de afectări congenitale sau valvulare, tratamentul aritmiilor prin ablație, angioplastie în caz de stenoze coronariene.
Însă, pentru majoritatea pacienților, tratamentul insuficienței cardiace presupune un control riguros al factorilor de risc. Modificarea stilului de viață și un tratament medicamentos adaptat, optim fac parte din controlul riguros. Uneori, utilizarea unor dispozitive care să susțină funcția corectă a inimii este necesară.
În ceea ce priveste stilul de viață, măsurile se referă la oprirea fumatului și a consumului de alcool. Scăderea ponderală, exercițiu fizic regulat, dieta hiposodată și o alimentație sănătoasă, săracă în grăsimi animale, bogată în fructe și legume este recomandată.
Medicație:
Se utilizează de obicei combinații de medicamente, dovedite a fi eficiente în acest tip de afecțiune. În mod normal, tratamentul se începe cu doze mici, urmând a fi crescute treptat, în funcție de anumiți parametrii. Se ajunge până la dozele maxim eficiente, cu efect pe supraviețuire, calitatea vieții, scăderea numărului de spitalizări. Pentru ca acest lucru să se întâmple, este necesară urmărirea periodică.
Frecvent se utilizeaza medicamente de tipul:
• Inhibitori de enzimă de conversie a angiotensinei (IECA) ex: prestarium, enap, enalapril, accupro, zomen, captopril, ramipril, tritace, cu mențiunea că medicul tău ar trebui să opteze pentru medicamentul potrivit, dovedit a fi util, la doze eficiente.
• Blocanți ai receptorilor de angiotensina II (sartani) cu acțiune similară cu IECA: telmisartan/micardis, valsartan, irbesartan, losartan, olmesartan
• Beta blocante : ex: carvedilol, metoprolol, bisoprolol, nebivolol.
• Inotrop pozitiv de tip digitalic – poate fi utilizat la anumiți pacienți, medicul tău va decide dacă este potrivit in cazul tău.
• Diuretice: ex: furosemid, nefrix, torasemida, bumetanida. Sunt principalele medicamente utilizate în cazul edemelor, dozele lor putând fi ajustate, la nevoie, la creștere ponderală rapidă ( cel mai probabil din cauza acumulării de lichid în organism, ceea ce poate duce la agravarea manifestărilor insuficienței cardiace; de ex: dispnee).
• Antagoniști ai aldosteronului: spironolactona, eplerenona
• Inotropi: utilizați în cazuri severe cu administrare intravenoasă, pentru a menține activitatea de pompă a inimii și valori normale ale tensiunii arteriale, mai ales atunci când nu se obține răspuns cu terapie clasică.
Sfatul medicului
Cel mai probabil doctorul îți va prescrie o asociere de mai multe medicamente dintre cele prezentate mai sus. La acestea se pot adăuga și alte medicamente pentru controlul simptomelor sau al factorilor de risc.
Aceste tratamente nu sunt însă lipsite de efecte secundare, unele potențial fatale. Din acest motiv se impune efectuarea periodică a unor teste de laborator care urmăresc funcția renală. Spre exemplu, ionograma (nivelul de sodium si potasiu) și hemograma (numărul principalelor elemente sanguine). De asemenea, funcția hepatică (transaminaze). Pentru a fi eficient, un tratament trebuie să fie corect și complet. Pentru ca acest lucru să fie posibil, este necesară urmărirea periodică, controlul datelor de laborator, dar și al altor constante personale (precum greutate, tensiune arterială, frecvența cardiacă, diureza – cantitatea de urină pe 24 de ore).
În afara tratamentului medicamentos, există și o serie de măsuri terapeutice moderne, de tip intervențional sau chirurgical, fie în scop curativ, fie pentru a îmbunătăți prognosticul insuficienței cardiace.
Astfel, în anumite situații se poate indica tratament chirurgical de tip by-pass aorto-coronarian. Tot chirurgical se pot corecta și leziuni ale valvelor inimii sau diferite defecte congenitale, acestea din urmă putând fi abordate și intervențional. De exemeplu, închiderea cu dispozitive de tip umbreluță a DSA sau foramen ovale, sau implantare de dispozitive în caz de persistență de canal arterial.
Uneori, susținerea funcție de pompă poate fi realizată sau menținută prin implantarea unor dispozitive la nivel cardiac, de tipul:
• Defibrilator cardiac implantabil
– dispozitiv asemănător unui pacemaker care presupune un generator implantat sub pielea toracelui, în partea stângă, deasupra mușchiului pectoral. La acest generator se conectează sonde care vor fi fixate intracardiac. Scopul lor este de a monitoriza ritmul cardiac prin administrare de șoc intern sau prin stimularea bătăilor inimii ( acestea realizându-se prin intermediul sondelor). Astfel tratează tulburările de ritm sau opririle cardiace, care pot pune viața în pericol.
• Terapia de resincronizare cardiacă (CRT) sau pacing biventricular
– în acest caz, sondele vor fi localizate la nivelul ambilor ventriculi, astfel încât contracția lor să fie coordonată, cât mai aproape de cea a unei inimi normale, așa încât să se mențină pompa cardiacă.
• Dispozitive de asistare ventriculară
– sunt dispozitive care se montează fie la nivelul toracelui, fie la nivel abdominal, atașate de o inimă mult prea afectată, pentru a o ajuta să realizeze funcția de pompă. Este, de obicei, un pas premergător transplantului cardiac sau ca o alternativă la transplant la cei care nu sunt candidați pentru acest tip de intervenție.
• Transplantul cardiac
– la cei la care tratamentele clasic și cel modern nu mai sunt suficiente pentru controlul insuficienței cardiace, în cazuri selecționate, extrem de severe, ținând cont de o serie de criterii foarte stricte.
Modificarea stilului de viață
• Oprirea fumatului: fumatul este asociat cu bolile coronarelor, dar și ale altor vase, cu hipertensiunea arterială, scade cantitate de oxigen în sânge, crește frecvența cardiacă. În plus, reprezintă contraindicație pentru transplantul cardiac.
• Cântărire zilnică: în fiecare dimineață, după urinat, înainte de micul dejun sau de administrare de lichide. O creștere ponderală rapidă poate sugera acumulare lichidiană și risc de decompensare cardiacș, care poate necesita ajustarea tratamentului.
• Restricție sodată: sarea în exces favorizează retenția apei în organism și apariția edemelor. Se recomandă un consum de 2-3 g de sare pe zi. Aceasta cantitate este conținută în alimentele obișnuite. Nu utilizați substituenți de sare în exces.
• Menținerea unei greutăți optime: scădere ponderala în caz de greutate excesivă.
• Dieta săracă în grăsimi saturate, grăsimi de tip trans și colesterol. Se recomandă grăsimi nesaturate, acizi de tip omega 3 și omega 6, grăsime de pește.
• Evitarea consumului excesiv de alcool
• Limitarea aportului de lichide în cazul insuficienței cardiace severe, la recomandarea medicului.
• Exercițiu fizic regulat există programe corespunzătoare pentru pacienții cu insuficiență cardiacț, pentru a promova un stil de viață activ, dar care să nu suprasolicite inima suplimentar.
• Reducerea stressului pe cât posibil.
• Somn odihitor
Complicații insuficiență cardiacă
- afectare renală – mergând până la insuficiența renală. Prin scăderea fluxului sanguin renal se produce deteriorare renală, cu consecințe severe în lipsa tratamentului adecvat. Se poate ajunge la dializa. În plus, tratamentul recomandat în insuficiența cardiacă poate avea consecințe pe funcția renală, de aceea necesită urmărire strictă periodică.
- afectare valvulară – prin dilatarea inimii sau prin creșterea presiunii în interiorul cavităților cardiace se poate ajunge la disfuncții valvulare de tip insuficiență, întrucât valvele nu se vor putea închide complet
- disfuncție hepatică – se produce staza hepatică ceea ce duce la creșterea presiunii la nivelul ficatului și secundar suferință hepatică.
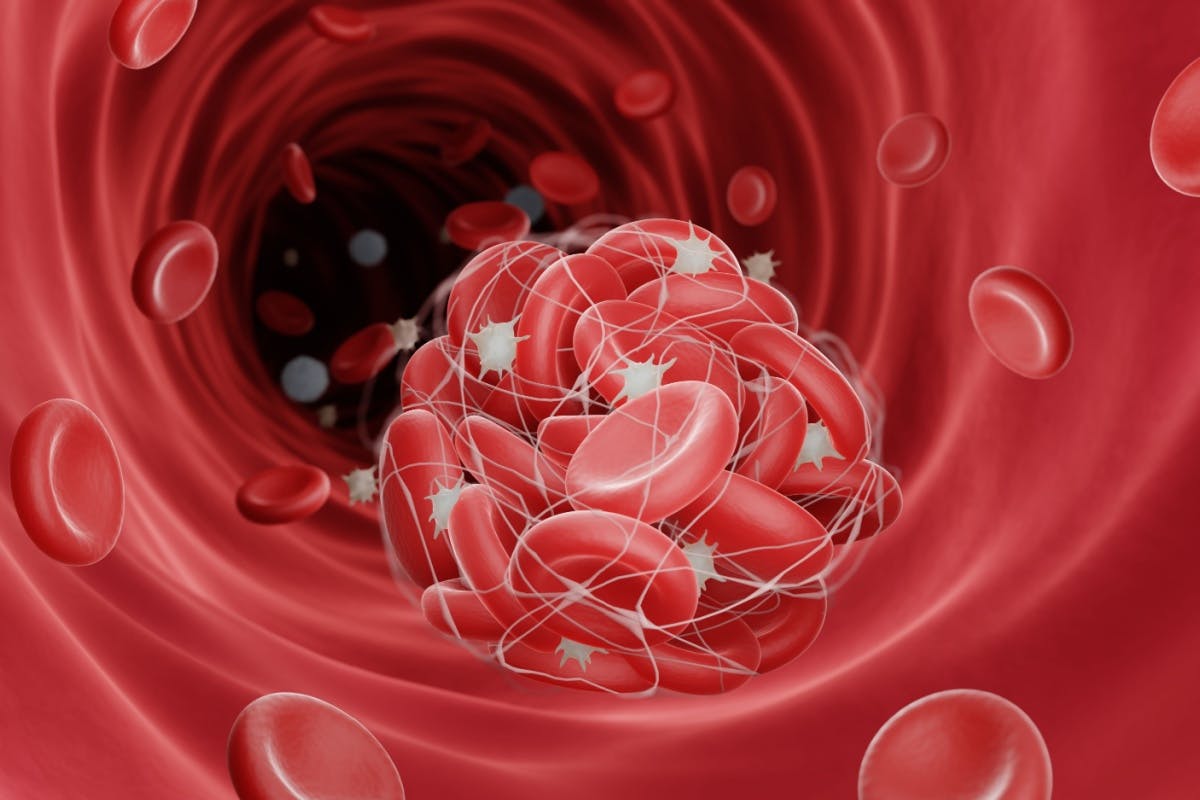
- accident vascular cerebral – prin dilatarea inimii și afectarea contracției cardiace, sângele poate stagna, ceea ce favorizează formarea trombilor (cheaguri de sânge). Aceștia pot să ajungă însă în circulație, inclusiv la nivel cerebral, producând AVC.
În anumite situații, simptomele și funcția cardiacă se pot îmbunătăți cu tratament corespunzător. Totuși, nu trebuie neglijat faptul ca insuficiența cardiacă este o afecțiune cu potențial letal. Unii pacienți pot dezvolta afectare severă cardiacă, care poate necesita terapii extreme. Printre acestea, sunt incluse transplantul cardiac sau asistarea artificială cu dispozitive care suplinesc funcția inimii.
La ARES vei beneficia de tratamente moderne ale afecțiunilor care stau la baza insuficienței cardiace (de tipul defectelor cardiace congenitale, bolilor coronariene) sau al complicațiilor insuficienței cardiace (implantare de dispozitive de tip stimulator cardiac, defibrilator, terapie de resincronizare cardiacă).
Distribuie:
Articole din categoria Cardiologie clinica
Articole mai noi
- Premieră națională în cardiologia structurală: primul implant Valve-in-Ring cu tehnica BATMAN la un pacient cu regurgitare mitrală severă
- Bolile de inimă în timpul sarcinii: Sfaturi pentru monitorizarea sănătății cardiovasculare
- Comparație între intervențiile tradiționale și cele microinvazive: Care sunt beneficiile pentru pacienți?
- Toracoscopia de diagnostic: ce este, când se recomandă și ce trebuie să știi înainte de intervenție
- Cum se decide între bypass și angioplastie? Rolul diagnosticului imagistic și al echipei multidisciplinare
Articole mai vechi
- Fibromul uterin - cauze, simptome, riscuri si tratament
- Despre Coronarografie - ce este și cât durează o astfel de procedură?
- Fibromul Uterin - responsabil de creșterea în greutate?
- Dr. Alexandra Postu: Cum tratăm infarctul miocardic acut prin cardiologie intervențională?
- Colaborare pentru inimi - Centrele Ares si Spitalul Monza