Stenoza pulmonara periferica / Tratament ingustare artera pulmonara
| Anestezie | generală |
| Durată procedură | 30-60 min |
| Durată spitalizare | 24 h |
Distribuie:
Cuprins
Generalități despre stenoza pulmonară periferică
Stenoza pulmonară periferică constă în îngustarea unei sau mai multor porțiuni la nivelul arterei pulmonare sau ramurilor acesteia. Este o afecțiune diferită de stenoză valvei pulmonare sau a venelor pulmonare.
SPP poate cauza obstrucție la nivelul trunchiului arterei pulmonare, la bifurcația acestuia sau la nivelul celor două ramuri: dreapta și stânga. Poate fi regăsită la un singur nivel sau în mai multe segmente (situația cea mai frecventă).
De asemenea, se poate asocia cu mai multe anomalii congenitale cardiace: stenoza valvei pulmonare, defect septal atrial, defect septal ventricular, persistența de canal arterial și, apare în 20% din cazurile de tetralogie Fallot. Poate fi și o consecință a lipsei congenitale a valvei pulmonare.
Se întâlnește și în alte afecțiuni, fie genetice, fie dobândite: rubeola, sindrom Noonan, sindrom Ehlers-Danlos, sindrom Williams, sindrom Alagille.
Uneori se poate evidenția o dilatație imediat după stenoză – situație întâlnită mai ales atunci când segmentul afectat este de dimensiuni mici, pe când în stenozele lungi sau în cazul arterelor hipoplazice (de calibru redus difuz) acest aspect poate lipsi.
Este o afecțiune care progresează, astfel că simptomele se pot agrava în timp. Mulți copii cu stenoză ușoară sunt asimptomatici. Acești copii au în general o cantitate mai mică de oxigen în sânge, ceea ce face ca inima să fie suprasolicitată cu scopul de a asigura oxigenarea adecvată.
Artera pulmonară:
• transportă sângele sărac în oxigen de la inimă la plămâni
• trunchiul arterei pulmonare pornește din ventriculul drept și se împarte în cele două artere pulmonare: dreapta și stânga, fiecare ajungând în plămânul corespunzător.
Cauzele stenozei pulmonare periferice
Cel mai adesea SPP este un defect congenital, mai rar este o afecțiune dobândită. Apare în situații precum:
• complicație a tetralogiei Fallot – asociere de 4 defecte cardiace (defect septal ventricular, hipertrofie de ventricul drept, stenoză pulmonară, aortă „călare”pe septul interventricular)
• în cadrul unor defecte genetice: sindroamele Noonan, Williams, Alagille
• în cazul condiției de tip „trunchi arterial”
• absența valvei pulmonare (atrezie pulmonară)
• stenoza valvei pulmonare
• în caz de persistență de canal arterial
• secundar unor infecții (de ex: rubeola congenitală).
Simptome
Majoritatea copiilor cu forme ușoare sunt asimptomatici – prezintă însă la examenul clinic obișnuit un suflu cardiac.
Așa cum am precizat anterior, SPP progresează în timp, așa că acești copii pot prezenta;
• oboseală
• dispnee (respirație dificilă)
• ritm cardiac accelerat
• edeme ale picioarelor, gleznelor
• edem al feței, abdomenului.
Observarea simptomelor de acest tip impune un consult de specialitate.
Diagnostic
Prezența un sufluc cardiac la examenul clinic obișnuit al copilului poate orienta diagnosticul. Uneori, aceste defecte pot fi evidențiate încă din viața intrauterină.
Imagistica are un rol important:
• radiografia toracică
• electrocardiograma – poate arăta aritmii cardiace se poate efectua și EKG de efort, care arată raspunsul inimii în timpul stresului (efortului)
• ecografia cardiacă – evidențiază anomaliie cardiace asociate, stenoza pulmonară
• imagistica prin rezonanța magnetică și computer tomografia
• cateterismul cardiac – este utilă pentru diagnostic, aprecierea gradului de obstrucție, evaluarea ventriculului drept și a arterei pulmonare, excluderea sau confirmarea altor afecțiuni cardiace
• angiografia pulmonară – presupune injectare de substanță de contrast pentru a evidenția anatomia arterei pulmonare și a ramurilor ei
• teste de perfuzie pulmonară, respectiv teste de ventilație-perfuzie care arată cât de bine trec aerul și sângele în plămâni.
Indicații
Întrucât acești copii au de obicei sânge sărac în oxigen și, întrucât boala se poate manifesta diferit, cel mai important este să vă adresați unui medic specialist, care vă poate îndruma corespunzător în vederea unui tratament adecvat.
În cazul formelor ușoare-moderate, de cele mai multe ori este suficientă urmărirea periodică prin examen clinic și ecografie cardiacă.
Tratament medicamentos:
Nu este curativ, dar poate ajuta la ameliorarea simptomelor. Astfel, diferite medicamente pot fi prescrise pentru:
1. menținerea funcției normale a inimii
2. controlul tensiunii arteriale
3. prevenția aritmiilor.
De asemenea, acești copii necesită tratament antibiotic în anumite situații (de ex. intervenții stomatologice, anumite intervenții chirurgicale) pentru a preveni complicații infecțioase care pot implica anumite structuri cardiace (endocardita infecțioasă).
Tratamentul intervențional:
În acest caz se utilizează catetere care, pe cale venoasă sau arterială, ajung la nivelul stenozei și permit corectarea acesteia. Se utilizează tehnici de tipul: dilatație cu balon, dilatație și implantare de stent, dispozitive „Cutting Ballon”.
E important de precizat că mulți copii necesită mai multe intervenții pe măsură ce cresc. Pe de altă parte, tratamentul intervențional este minim invaziv, asociază riscuri scăzute, iar rezultatele sunt în general foarte bune. În plus, copiii supuși unei asemenea intervenții pot trăi absolut normal, fără restricții.
Așa cum am spus anterior, gradul de afectare poate varia în cadrul SPP, de aceea medicul specialist este cel care vă poate orienta cel mai bine privind tratamentul optim.
Cum te pregătești pentru intervenție?
 1. Vei efectua analize de sânge
1. Vei efectua analize de sânge 2. Vei efectua o electrocardiogramă și o ecografie cardiacă.
2. Vei efectua o electrocardiogramă și o ecografie cardiacă. 3. Nu vei mânca și nu vei bea apă
3. Nu vei mânca și nu vei bea apă
Cât durează internarea?
Tratamentul intervențional prezintă avantajul unei internări de scurtă durată și a unei perioade scurte de convalescență. Perioada de internare variază între 24 și 48 de ore, timp în care vor fi efectuate analize, investigații și procedura de diagnosticare și tratament. Te poți întoarce la viața ta, în numai câteva zile.
Riscuri
Complicațiile sunt rare și sunt evitate printr-o pregătire și supraveghere corespunzătoare. Complicațiile posibile includ:
- reacții alergice la administrarea substanței de contrast, inclusiv insuficiența renală
- reacții la compușii anestezici
- fistule arteriovenoase la locul puncției
- sângerări la locul puncției
- febră
- cefalee (durere de cap), migrenă
- infecții
- embolie gazoasă
- aritmii cardiace
- foarte rară – perforație cardiacă și tamponadă cardiacă
- infarct miocardic
- accident vascular cerebral
- insuficiență valvei pulmonare
- restenoza
- datorită creșterii, de obicei sunt necesare mai multe intervenții până la vârsta de adult.
Ce se întâmplă în timpul procedurii
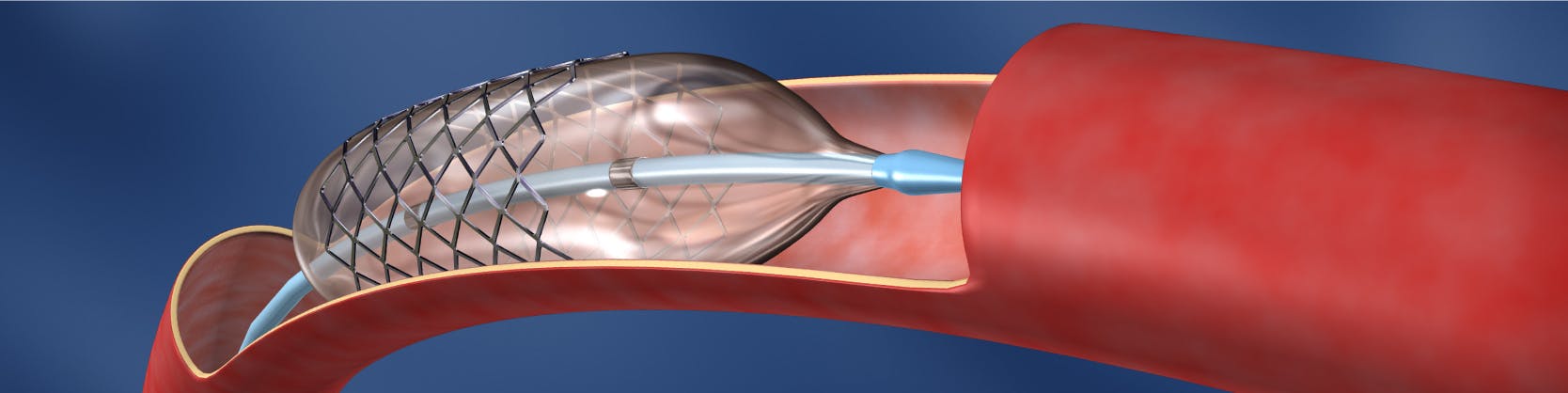
Procedura se efectuează în laboratorul de angiografie și de obicei, se practică sub anestezie generală. După asepsia locală, medicul intervenționist va efectua mici incizii la nivelul canalului inghinal ( la rădăcina coapsei) pentru a vizualiza vena femurală. La nivelul acestei mici incizii, sub ecran radiologic, se va introduce o teacă, ulterior pe teacă se introduc catetere până la nivelul ventriculului drept și ulterior până la nivelul porțiunii îngustate a arterei pulmonare sau a ramurilor acesteia. Se efectuează angiograme repetate, pentru a vizualiza stenoza și a verifica locul cateterului. Pe acest cateter se avansează un alt cateter cu balon detașabil, până în apropierea stenozei. Balonul va fi umflat la nivelul îngustării, care va fi mărită progresiv, îndepărtându-se astfel stenoza. Ulterior balonul se dezumfla și este îndepărtat. (procedura cunoscută sub numele de dilatare cu balon).
Dilatare cu balon si implantare de stent
Efectele dilatării cu balon pot fi amplificate dacă după procedeul de dilatare se montează un stent (tub mic, subțire) la nivelul zonei afectate, pentru a menține vasul deschis.
Dispozitivul Cutting ballon
Este un dispozitiv mai nou care repreinztă un balon cu 3-4 lame mici atașate, cu ajutorul cărora se fac mici incizii la nivelul stenozei. Se poate utiliza mai ales în cazul în care procedura simplă de dilatare nu a fost eficientă.
Ce se întâmplă după procedură?
 1. Vei bea cel puțin 2 litri de apă, pentru a elimina substanța de contrast.
1. Vei bea cel puțin 2 litri de apă, pentru a elimina substanța de contrast. 2. Ti se va monitoriza pulsul, tensiunea și temperatura
2. Ti se va monitoriza pulsul, tensiunea și temperatura 3. Vei fi externat
3. Vei fi externat
Ce trebuie să faci după ce ieși din spital?
Dacă ai trecut printr-o astfel de procedură, este important să revii la control așa cum ți-a recomandat medicul tău și să respecți tratamentul indicat de acesta. Îți poți relua activitatea imediat.
Se fac evaluări periodice (examen clinic, electrocardiogramă și ecografie) la 1 lună, 6 luni și respectiv 1 an după intervenție, ulterior anual.
Sunt indicate imunizarea copiilor și profilaxia endocarditei.
Activitatea fizică moderată nu trebuie limitată.
Distribuie:
Locații MONZA ARES în care se efectuează Stenoza pulmonara periferica / Tratament ingustare artera pulmonara
Procedurile Noastre
- Investigații cardiologie
- Investigații neurologie
- Bolile valvelor și ale vaselor inimii
- Aritmii cardiace
- Defecte (malformații) cardiace din naștere
- Bolile vaselor de sânge
- Fibroid Center
- Boli oncologice si tratamente tumorale
- Bolile valvelor și ale vaselor inimii la copii
- Boli ale aparatului genital masculin
- Boli cerebrale și ale coloanei vertebrale
- Boli ale articulațiilor





