Tratament insuficiență mitrală - MitraClip
| Anestezie | locală/generală |
| Durată procedură | 1-3 h |
| Durată spitalizare | 24-48 h |
Distribuie:
Cuprins
Insuficiența mitrală și regurgitarea mitrală
La nivel global, insuficiența mitrală sau regurgitarea mitrală este una dintre cele mai frecvente afectări valvulare. De regulă, dacă este vorba de o formă ușoară, tratamentul nu este întotdeauna necesar. Forma severă a acestei valvulopatii poate cauza însă, în lipsa tratamentului adecvat, tulburări de ritm cardiac (aritmii) sau insuficiență cardiacă. Pentru tratarea acestei probleme se recurge, de obicei, la intervenții chirurgicale pentru înlocuirea sau repararea valvei mitrale.
Tratamentul chirurgical nu reprezintă însă o opțiune pentru toți pacienții, în special pentru cei cu risc operator crescut. În astfel de cazuri este recomandată procedura MitraClip. [1][3]
Ce reprezintă procedura MitraClip?
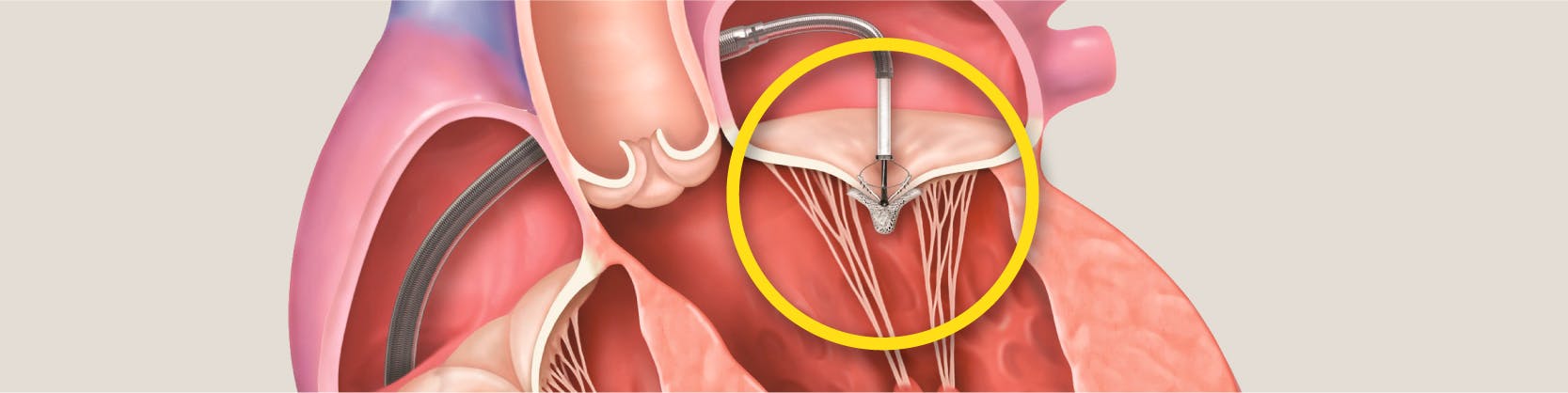
Procedura MitraClip este o procedură intervențională minim invazivă recomandată în tratamentul regurgitării mitrale. Pe scurt, presupune introducerea până la nivelul valvei mitrale a unui dispozitiv sub formă de clips al cărui rol este acela de a uni porțiunile mijlocii ale foițelor valvei, creând un orificiu mitral dublu.
Acest lucru îi va permite valvei mitrale să se închidă mai bine și va reduce regurgitarea, restabilindu-se fluxul astfel sangvin normal. [4]
Ce este insuficiența mitrală?
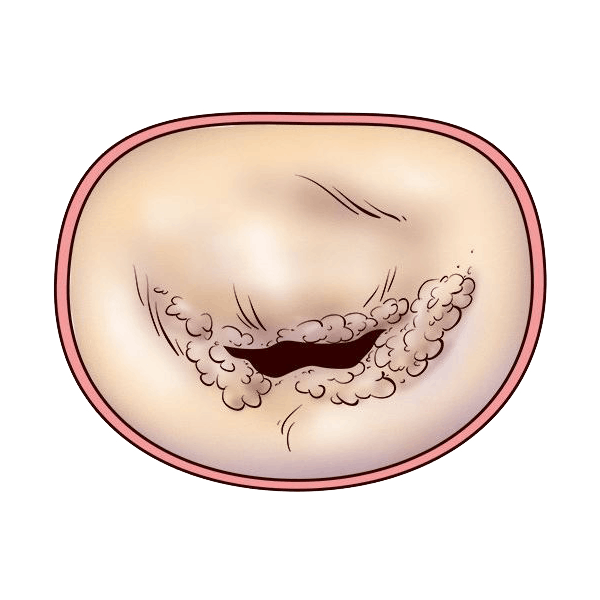
Inima noastră are patru camere: atriul stâng, atriul drept, ventriculul stâng și ventriculul drept. Valva mitrală este situată între atriul stâng și ventricul stâng și, în mod normal, ar trebui să acționeze ca un pasaj unidirecțional care să îi permită sângelui să treacă din atriu în ventricul, nu și înapoi. [2]
Regurgitarea mitrală (RM) este o afecțiune care se caracterizează prin închiderea incompletă a valvei mitrale, ceea ce face ca o parte din sânge să se reîntoarcă din ventriculul stâng în atriul stâng. În consecință, pentru a asigura volumul necesar de sânge în corp, inima va fi suprasolicitată și, în timp, pacientul va resimți oboseală, dispnee (respirație dificilă) și se va ajunge la agravarea insuficienței cardiace. RM este una dintre cele mai frecvente afecțiuni valvulare.
Există mai multe grade de regurgitare mitrală, în funcție de severitatea sa, insuficiența mitrală de gradul 1 și insuficiența mitrală de gradul 2 fiind cele mai ușoare. În cazul formelor ușoare, nu este întotdeauna necesar să se intervină pentru tratarea regurgitării mitrale. De exemplu, dacă ai fost diagnosticat cu insuficiență mitrală de gradul I, tratamentul recomandat ar putea presupune monitorizarea atentă a acesteia și schimbarea stilului de viață.
Cât poți trăi cu insuficiență mitrală depinde de cauza sa, stadiul și severitatea bolii și de cât timp este prezentă această problemă. [3]
Care sunt cauzele regurgitării mitrale?
Cauzele regurgitării mitrale pot fi ischemice (ca și consecință a bolilor cardiace ischemice) sau non-ischemice. Acestea din urmă pot fi:
- Cauze degenerative (boli mixomatoase, degenerarea foițelor mitralei – două la număr: anterioară și posterioară, calcificarea inelului mitral);
- Endocardită;
- Boli reumatismale;
- Afecțiuni congenitale;
- Cardiomiopatii;
- Boli inflamatorii;
- Afecțiuni induse de medicamente;
- Traumatisme.
Principalele cauze ale bolii de valvă mitrală rămân însă:
- Prolapsul de valvă mitrală (PVM);
- Bolile ischemice;
- Sindromul Marfan;
- Reumatismul articular.
Regurgitarea mitrală mai poate fi degenerativă sau funcțională. Regurgitarea degenerativă este denumită și insuficiența mitrală primară și se datorează afectării foițelor valvei mitrale. Insuficiența mitrală funcțională, denumită și secundară, este provocată de mărirea cordului (așa cum se poate întâmpla în infarctul miocardic, insuficiență cardiacă, unele cardiomiopatii).
Pacienții pot fi asimptomatici sau se pot prezenta cu semne și simptome ale insuficienței cardiace, precum dispnee sau edem pulmonar. Pe termen lung poate duce la dilatarea ventriculului stâng, fibrilație atrială, insuficiență cardiacă.
Care sunt cauzele regurgitării mitrale?
Cauzele regurgitării mitrale pot fi ischemice (ca și consecință a bolilor cardiace ischemice) sau non-ischemice. Acestea din urmă pot fi:
- Cauze degenerative (boli mixomatoase, degenerarea foițelor mitralei – două la număr: anterioară și posterioară, calcificarea inelului mitral);
- Endocardită;
- Boli reumatismale;
- Afecțiuni congenitale;
- Cardiomiopatii;
- Boli inflamatorii;
- Afecțiuni induse de medicamente;
- Traumatisme.
Principalele cauze ale bolii de valvă mitrală rămân însă:
- Prolapsul de valvă mitrală (PVM);
- Bolile ischemice;
- Sindromul Marfan;
- Reumatismul articular.
Regurgitarea mitrală mai poate fi degenerativă sau funcțională. Regurgitarea degenerativă este denumită și insuficiența mitrală primară și se datorează afectării foițelor valvei mitrale. Insuficiența mitrală funcțională, denumită și secundară, este provocată de mărirea cordului (așa cum se poate întâmpla în infarctul miocardic, insuficiență cardiacă, unele cardiomiopatii).
Pacienții pot fi asimptomatici sau se pot prezenta cu semne și simptome ale insuficienței cardiace, precum dispnee sau edem pulmonar. Pe termen lung poate duce la dilatarea ventriculului stâng, fibrilație atrială, insuficiență cardiacă.

Care sunt simptomele regurgitării mitrale?
Semnele și simptomele insuficienței mitrale depind de severitatea și de rapiditatea instalării acestei condiții. Printre cele mai frecvente se numără însă:
- Oboseala puternică (oboseală la efort);
- Palpitații (ai senzația că inima ta bate prea repede sau prea tare ori că sare o bătaie; de obicei, acest lucru tinde să se întâmple când stai întins pe partea stângă);
- Amețeli bruște;
- Lipotimii (leșinuri);
- Suflu cardiac (sunet provocat de fluxul sangvin, ce poate fi perceput cu ajutorul unui stetoscop);
- Dispnee (dificultăți de respirație);
- Aritmie;
- Umflarea gleznelor și picioarelor (edem). [3][2]
De cele mai multe ori, insuficiența mitrală este ușoară și progresează lent. De aceea, pot trece ani până la apariția simptomelor. Există și situații când afecțiunea se dezvoltă brusc (de ex. uneori în infarctul miocardic) și în acest caz, simptomele se instalează acut.
Diagnosticarea insuficienței mitrale
Procesul de diagnosticare a regurgitării mitrale începe cu anamneza și examenul clinic, urmate de unul sau mai multe teste și investigații. Printre cele mai comune se numără:
- Ecocardiografia - arată structura valvei mitrale și permite evaluarea fluxului sangvin; poate confirma diagnosticul de insuficiență mitrală și determina severitatea acesteia;
- Electrocardiografia - măsoară activitatea electrică a inimii și poate detecta tulburările de ritm cardiac asociate cu insuficiența mitrală;
- Radiografia - permite evaluarea dimensiunilor camerelor inimii;
- RMN - oferă imagini detaliate ale inimii și poate ajuta la obținerea mai multor informații privind severitatea insuficienței mitrale, dar și dimensiunea și funcția ventriculului stâng;
- Test de efort sau test de stres - arată modul în care inima funcționează în condiții de efort;
- Coronarografia - permite vizualizarea arterelor inimii, oferind informații importante despre structura și funcțiile acesteia. [3]
Cum te pregătești pentru Mitraclip?
 1. Vei face un examen clinic complet
1. Vei face un examen clinic complet 2. Vei face o radiografie toracică
2. Vei face o radiografie toracică 3. Vei face o tomografie computerizată cu substanță de contrast
3. Vei face o tomografie computerizată cu substanță de contrast 4. Vei face un set complet de analize de sânge
4. Vei face un set complet de analize de sânge 5. Vei face o coronarografie
5. Vei face o coronarografie 6. Vei face o ecografie doppler a arterelor de la nivelul gâtului
6. Vei face o ecografie doppler a arterelor de la nivelul gâtului 7. Vei elimina orice potențial focar infecțios: infecții ORL, stomatologice, etc
7. Vei elimina orice potențial focar infecțios: infecții ORL, stomatologice, etc
Care sunt riscurile MitraClip?
Complicațiile sunt rare și pot fi evitate printr-o pregătire și supraveghere corespunzătoare. Complicațiile posibile includ:
- Reacții alergice la administrarea substanței de contrast, inclusiv insuficiența renală;
- Reacții la compușii anestezici;
- Fistule arteriovenoase la locul puncției;
- Sângerări, hematom la locul puncției;
- Febră;
- Cefalee (durere de cap), migrenă;
- Infecții la locul puncției;
- Embolie gazoasă;
- Aritmii cardiace;
- Accident ischemic tranzitor sau accident vascular cerebral – risc redus prin efectuarea de rutină a ETE, pentru a exclude prezența trombilor;
- Stenoza mitrală iatrogenă – deși nu a fost descrisă în studiile efectuate, există un risc al acestei complicații, mai ales în cazul implantării mai multor clipuri;
- Creșterea gradientului transmitral;
- Defect septal atrial iatrogen;
- Intervenție chirurgicală necesară în cazul rezultatelor nesatisfăcătoare – rar.
Ce se întâmplă în timpul procedurii MitraClip?
Procedura se efectuează în sala de angiografie.
- Se pregătește locul de abord prin îndepărtarea părului din zona inghinală, se efectuează asepsia locală și se administrează tratament anticoagulant;
- Medicul intervenționist va efectua mici incizii la nivelul canalului inghinal (la rădăcina coapsei) pentru a vizualiza artera femurală;
- La acest nivel, se va introduce o teacă; ulterior, pe teacă se introduce un cateter-ghid;
- Cateterul va fi ghidat sub ecran radiologic până la nivelul atriului drept;
- Se injectează substanța de contrast și se efectuează angiograme repetate, pentru a vizualiza regurgitarea mitrală și pentru a verifica locul cateterului;
- Va fi puncționat septul interatrial (puncție transseptală);
- Se va introduce un nou cateter pe ghid, care va fi fixat în una din cele patru vene pulmonare (vena pulmonară superioară);
- Pe cateterul-ghid va fi introdus în atriul stâng sistemul MitraClip, care, sub imagine ecografică, va fi poziționat la nivelul valvei, astfel încât „brațele” dispozitivului să fie dispuse perpendicular pe foițele valvei;
- Odată ce s-a poziționat optim, dispozitivul MitraClip va fi avansat către ventriculul stâng; când medicul confirmă poziția corectă și reducerea regurgitării, clipul va fi detașat; în caz contrar va fi repoziționat; uneori, poate fi montat un al doilea clip;
- Se scot cateterele și tecile arteriale, iar la locul de puncție se realizează compresia arterei folosite ca abord; pentru a se obține compresia, se pune un pansament compresiv ce trebuie păstrat timp de 24 de ore pentru a se evita sângerările; în ambele cazuri de abord, este indicată păstrarea repausului la pat; în anumite situații, există indicația de a monta un sistem hemostatic la nivelul puncției femurale; acesta se montează în sala de angiografie, imediat după terminarea intervenției; AngioSeal este mic dop de colagen și se introduce în interiorul arterei femurale, având ca efect obținerea hemostazei în doar două ore; astfel, pacientul își poate mișca piciorul în voie și se poate ridica din pat.
Ce se întâmplă după procedura MitraClip?
După terminarea procedurii:
 1. Vei fi transferat în unitatea de ATI
1. Vei fi transferat în unitatea de ATI 2. În primele 24-48 ore vei fi extubat
2. În primele 24-48 ore vei fi extubat 3. Vei primi un tratament medicamentos
3. Vei primi un tratament medicamentos 4. Vei fi supus mai multor examene clinice și investigații
4. Vei fi supus mai multor examene clinice și investigații
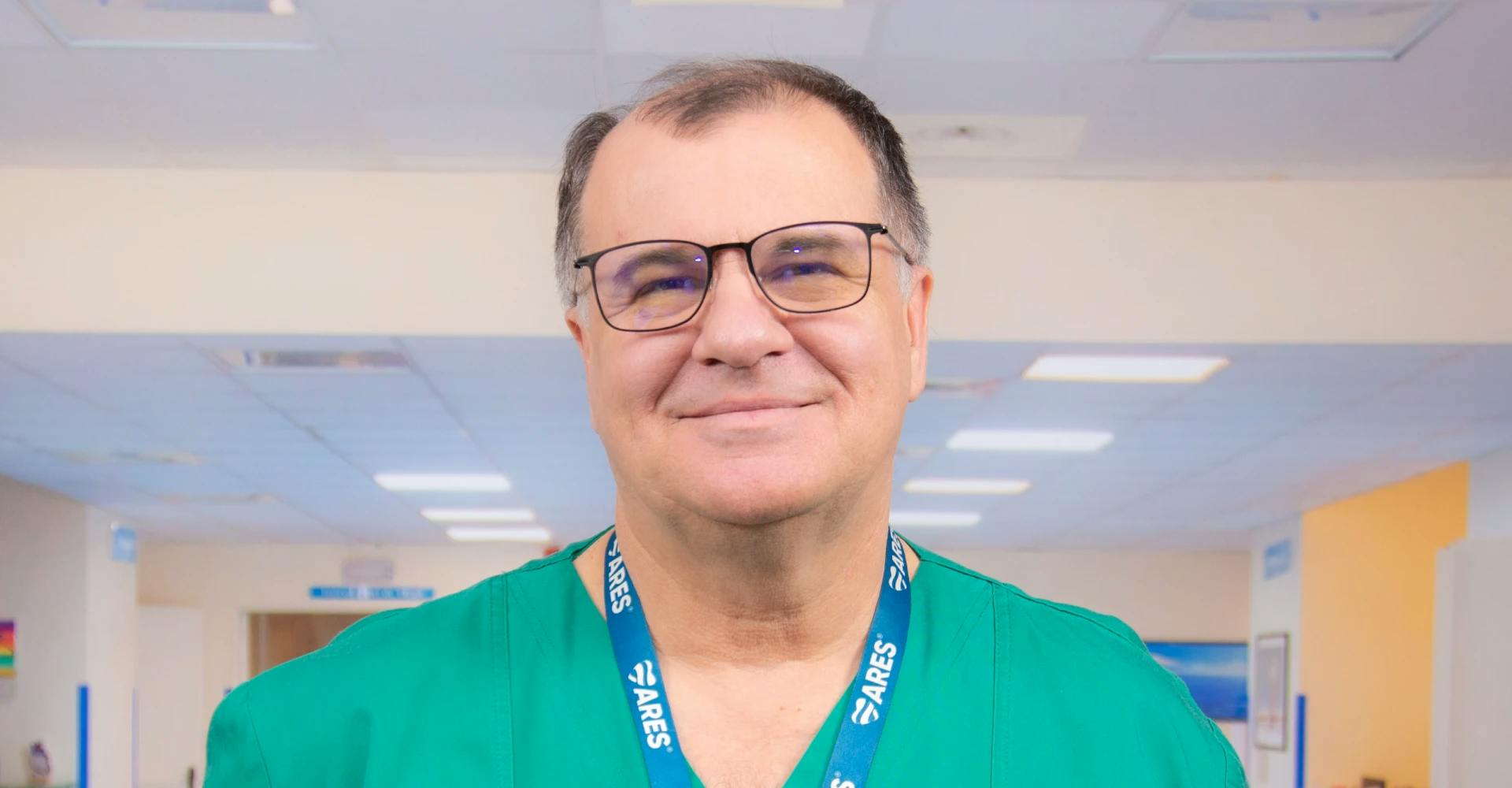
Doctori care efectuează tratamentul insuficienței mitrale la MONZA ARES
Cazuri tratate la MONZA ARES
Locații MONZA ARES în care se efectuează Mitraclip
Întrebări frecvente
Cât durează internarea după tratamentul MitraClip?
Comparativ cu chirurgia cardiacă, procedura Mitraclip are avantajul unei recuperări rapide și a unei scurte durate de spitalizare. Durata de spitalizare este, în general, sub o săptămână, dacă evoluția post intervenție este favorabilă și fără complicații. În mod normal, ar trebui să poți pleca acasă după 2-3 zile.
Ce dispozitive medicale sunt folosite pentru procedura MitraClip?
Sistemul MitraClip reprezintă un cateter ghid și un sistem care conține la capătul său clips-ul și permite delivrarea lui la nivelul foițelor valvei. Clips-ul are două „brațe” fiecare cu o porțiune centrală („gripper”) care, prin unire, facilitează unirea celor două foițe ale valvei mitrale.

Ce trebuie să faci după ce ieși din spital?
Dacă ai fost supus unei proceduri MitraClip, trebuie să revii la controlul cardiologic la o lună, la trei luni și apoi o dată la șase luni, în funcție de evoluție. Imediat după externare vei face recuperare fizică. Vei urma un tratament cu aspirină și antiagregant plachetar timp de aproximativ trei luni, la indicația medicului.
Care este prețul procedurii MitraClip?
Colegii noștri îți stau la dispoziție pentru a-ți răspunde la toate întrebările referitoare la această procedură, inclusiv cele privind prețul acesteia. Dacă vrei să știi care este prețul procedurii MitraClip sau care este prețul unei operații a valvei inimii, tot ce trebuie să faci este să ne suni sau să completezi formularul disponibil pe site și vei contactat în cel mai scurt timp de către unul dintre consultanții noștri.
Insuficiența mitrală este o afecțiune ce trebuie monitorizată constant și care, în lipsa tratamentului adecvat, poate duce la apariția unor probleme grave de sănătate. Tratamentul standard pentru regurgitarea mitrală este cel chirurgical, dar acesta nu este o opțiune potrivită pentru toți pacienții și presupune mai multe riscuri. În astfel de cazuri, este de preferat să se apeleze la procedura MitraClip, care permite tratarea insuficienței mitrale pe cale minim invazivă.
Bibliografie:
- Fiorilli, Paul N., et al. „Transcatheter Mitral Valve Replacement: Latest Advances and Future Directions.” Annals of Cardiothoracic Surgery, vol. 10, no. 1, Jan. 2021, pp. 85–95, www.ncbi.nlm.nih.gov/pmc/articles/PMC7867435/, 10.21037/acs-2020-mv-21. Accessed 29 Sept. 2022.
- „What Is Mitral Valve Regurgitation?” WebMD, WebMD, 15 Sept. 2016, www.webmd.com/heart-disease/what-is-mitral-valve-regurgitation. Accessed 29 Sept. 2022.
- „Mitral Valve Regurgitation - Symptoms and Causes.” Mayo Clinic, 2022, www.mayoclinic.org/diseases-conditions/mitral-valve-regurgitation/symptoms-causes/syc-20350178. Accessed 29 Sept. 2022.
- „Transcatheter mitral valve repair” Uptodate.com, 2022, www.uptodate.com/contents/transcatheter-mitral-valve-repair. Accessed 29 Sept. 2022.
Distribuie:
Locații MONZA ARES în care se efectuează Tratament insuficiență mitrală - MitraClip
Procedurile Noastre
- Investigații cardiologie
- Investigații neurologie
- Bolile valvelor și ale vaselor inimii
- Aritmii cardiace
- Defecte (malformații) cardiace din naștere
- Bolile vaselor de sânge
- Fibroid Center
- Boli oncologice si tratamente tumorale
- Bolile valvelor și ale vaselor inimii la copii
- Boli ale aparatului genital masculin
- Boli cerebrale și ale coloanei vertebrale
- Boli ale articulațiilor